This guide was prepared by a Task Force of the AES Practice Management Committee: Chair, Anup D. Patel, MD and members Rohit Das, MD, MPH, and Anu Venkat, MD, with input from committee members and recent AES telehealth webinar faculty experts, Marvin A. Rossi, MD, PhD and Edward "Rusty” J. Novotny, MD. The information was reviewed and approved by the committee and AES Council on Clinical Activities and complements the webinars and other telehealth information from other organizations and CMS, as referenced in the Additional Resources section.
Important: The Centers for Medicare and Medicaid Services (CMS) and states continue to adjust regulations regarding telehealth for Medicare. This Quick Guide is primarily a summary of selected points related to newly enacted temporary regulatory flexibility for Medicare during the COVID-19 emergency. The underlying regulatory landscape is complex, and this guide is not intended as a substitute for consulting primary CMS information sources. In addition, Medicaid and private payer requirements vary state-to-state. Providers should closely monitor CMS and state-specific information for evolving changes during and after the current COVID-19 situation. Several organizations monitoring Medicare and state requirements provide useful summaries and/or more detail. Please see the Additional Resources section for links to further information.
BACKGROUND
The Center for Medicare and Medicaid Services (CMS) has broadened access to Medicare telehealth services on a temporary and emergency basis under the 1135 waiver authority and Coronavirus Preparedness and Response Supplemental Appropriations Act. The waiver applies to Medicare across the country without regional restrictions. The blanket waiver means that providers do not need to apply for individual 1135 waivers for the covered provisions.
SELECTED PROVISIONS OF THE CURRENT 1135 WAIVER
The waiver offers providers flexibilities and alternatives to in-person care to ensure that Medicare beneficiaries, who are at a higher risk for COVID-19, are able to access the healthcare they need during the COVID-19 emergency without having to go to a doctor’s office or hospital. The waiver generally broadens access to telehealth services and broadens flexibility without regard to diagnosis.
Across State Lines: Effective March 6, 2020, under Section 1135 of the Social Security Act, the Secretary of Health and Human Services has issued a waiver to the requirements that physicians or other health care professionals hold licenses in the State in which they provide services if they have an equivalent license from another State (and are not affirmatively barred from practice in that State or any State a part of which is included in the emergency area).
The CMS waiver applies to Medicare services, but individual states may still require certain licensure standards, and other Medicaid and payer requirements vary state-to-state, as noted previously. (See Additional Resources section).
Patient and Provider Sites: Providers may provide telehealth services from their location (called the “Distant Site”), including home or clinic office. New under the 1135 waiver, patients may receive telehealth services in their homes (called the “Originating Site”); prior to the 1135 waiver, telehealth services received in patient homes was permitted only for very limited specific services.
Providers Types: Physicians, advanced practice providers, pharmacists, clinical psychologists, dieticians, and licensed social workers may offer telehealth services to their patients.
Types of Services: Under the 1135 waiver, Medicare began covering office, hospital, and other visits furnished via telehealth starting March 6, 2020. The coverage is for a specific set of services through telehealth and includes telemedicine evaluation and management (E/M) visits (common office visits), mental health counseling, and preventive health screenings.
Established Relationship: Under the provisions of the 1135 waiver, virtual office visits (telemedicine) are covered for both new patients and those having an established relationship with a practitioner. Previously applicable only to established patients in most circumstances, under the waiver E-Visits and Virtual Check-Ins are permitted for both new and established patients (see Table 1).
Consent: Providers must obtain consent prior to the telehealth interaction. This is typically done at the time the appointment is made. Consent can be obtained either in verbal or written form and should be documented in the clinical record.
Telemedicine versus Telehealth: Telehealth, telemedicine, and related terms generally refer to the exchange of medical information from one site to another through electronic communication to improve a patient’s health. There are important distinctions between the terms telemedicine and telehealth as used by CMS. Telehealth is the broader term and includes telemedicine.
Telehealth under Medicare applies to a pre-determined set of clinical services and includes both provider-patient and peer-to-peer interactions. Telemedicine is generally defined as a synchronous visit between a patient and provider rendered via video and audio communication and is sometimes called Video Telehealth. Similarly, Medicaid has described telemedicine as an electronic communication using interactive audio and video that seeks to improve a patient's health by permitting two-way, real-time interactive communication between the patient and the physician or practitioner, as a cost-effective alternative to the more traditional way of providing medical care via provider-patient in-person consultations or examinations.
Telehealth Platforms: A variety of telehealth platforms are available that may or may not be integrated with the electronic medical record. HIPAA-compliant platforms are preferred; however, under the emergency waiver non-HIPAA compliant platforms may be permitted if they are “non- public-facing,” as defined by CMS.
TYPES OF TELEHEALTH VIRTUAL HEALTH SERVICES
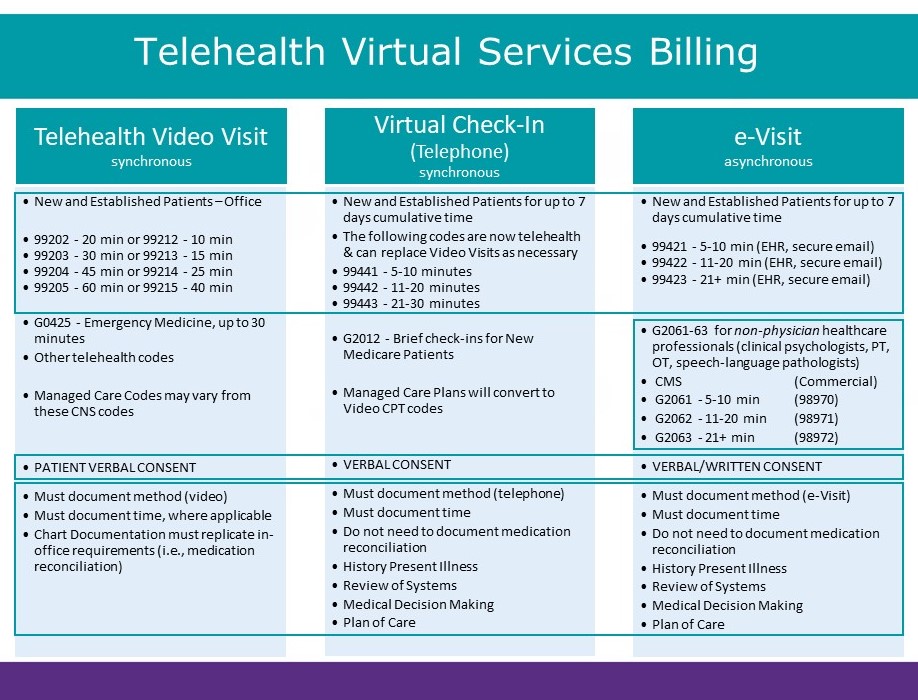
In recent COVID-19-related changes to telehealth regulations under the 1135 waiver, CMS expanded available Medicare telehealth services with a focus on three types of virtual health services physicians and other health care professionals can provide to patients. The three types of services, along with key billing information, are briefly summarized in Table 1, followed by more details and examples of each.
Table 1. Summary of Telehealth Virtual Services Billing Under 2020 CMS COVID-19 Waiver (May 2, 2020 update)
KEY POINTS: THREE TYPES OF TELEHEALTH VIRTUAL SERVICE UNDER THE 2020 CMS COVID-19 WAIVER
- Telehealth Visits – Synchronous virtual office visits between a provider and patient, previously required to use both audio and video, but under the 1135 waiver now may be telephone only
- Includes evaluation and management (E/M) visits (common office visits), mental health counseling and preventive health screenings
- CMS announced new flexibility on April 30, 2020, to allow telephone-only E/M telehealth visits, with corresponding telehealth video visit codes, retractive to March 1, 2020
- Previously, required video distinguished this type of telehealth type as "telemedicine"
- New patients and patients with established provider relationships
- No patient location restrictions, and not limited to rural health care
- Increased flexibility for this type of telehealth service is one of the most significant changes under the current CMS 1135 waiver for the COVID-19 emergency
- Covers services that otherwise do not fall under Virtual Check-ins (See Example 2 in the Additional Examples section), E-Visits (See Example 3 in the Additional Examples section) or Remote Monitoring (another type of telehealth service not addressed here).
- Example: The virtual equivalent of an in-person office visit. (See Example 2 and Example 3D in the Additional Examples section.)
- Virtual Check-ins – Short (5-10 min), synchronous, patient-initiated communications with a health care practitioner
- Typically telephone/audio only (so not considered “telemedicine”), but may include exchange of information through video or image
- Established and new patients (COVID-19 waiver adds new patients)
- Typically used to determine whether an E/M visit is needed.
- For reimbursement, communication should not be related to a medical visit within the previous 7 days and does not lead to a medical visit within the next 24 hours
- Example: A patient communicates about a new problem to determine if a longer visit is needed. If an actual visit takes place, then billing cannot occur for the virtual check-in. (See also Examples 3B and 3C in the Additional Examples section.)
- E-Visits – Non-face-to-face, asynchronous, patient-initiated communications through an online patient portal
- Typically conducted through messaging in an electronic health record
- Established and new patients (COVID-19 waiver adds new patients)
- Asynchronous distinguishes E-Visits from Video Telehealth Visits and Virtual Check-Ins
- For reimbursement, cumulative communications over a 7-day period, but no longer
- No location restrictions, and not limited to rural health care
- Example: Communications via MyChart for Epic users. (See also Example 3A in the Additional Examples section.)
ADDITIONAL EXAMPLES
- The medicine team contacts the epilepsy consult service for a 63-year-old man with a COVID-19 positive status who has a history of epilepsy. He is on valproate for his epilepsy. The patient had a seizure in the ICU, witnessed by the nurse. His VPA level is 38. His daughter states that he typically has levels in the 60s.
This patient may be suitable for interprofessional electronic health record assessment and management service where the neurologist will review the EMR, propose an intervention (supplemental valproate dosing) without physically seeing the patient. The likelihood is that the patient will not be seen again inpatient by neurology. If neurology sees the patient in person at a later stage, this code will not be reimbursed. - An 18-year-old boy with a first seizure contacts your office seeking to see an epileptologist.
In the setting of the COVID-19 pandemic the patient may be seen as a Video Telehealth Visit. Consent can be obtained and documented at the time the appointment is scheduled. The visit can be completed using a real-time audio-visual communication system. Since a physical examination cannot be completed, the visit would be billed using medical decision making or time. - A 43-year-old man contacts the medical office using the electronic medical record system’s e- messaging option stating that he has had a cluster of 4 seizures over the last two days. He has intractable epilepsy and typically has one seizure a week. He has been stable on his current medication for the last year. Three options exist:
- After reviewing his chart and communication, you realize that he has been sick with a mild fever during the time he had his flurry of seizures. Three years prior, he had a similar flurry of seizures with a mild URI. You write back to him providing reassurance but making no medication changes. This would be an e-Visit (codes 99421-99423).
- After reviewing the chart, you decide the patient needs a quick communication. This is a Virtual Check-in (G2012) to determine if an in-person visit is needed.
- After reviewing the chart, you decide you want to have a phone conversation with the patient to determine whether he is taking his medication regularly and determine what other issues may be involved. This would then be a Telephone visit that is categorized as a Virtual Check-in (99441-99443).
- Important Update: CMS announced April 30, 2020, that if the interaction is an evaluation and management visit, it may be billed as a virtual telehealth visit, with corresponding reimbursement, retroactive to March 1, 2020.
CONSULTATIVE PEER-TO-PEER SERVICES
Telehealth waiver provisions allow for billing of interprofessional (peer-to-peer) telephone/Internet/electronic health record assessment and management service provided by a consultative physician, including a verbal and written report to the patient’s treating/requesting physician or other qualified health care professional.
- Can be used in hospital to provide guidance to the requesting provider without having to have face to face contact with the patient (example: simple ASM management in COVID-19 patient).
- Best used for a one time consult where there is not a need to see the patient.
- 99446, Telephone/Internet Assessment,
5-10 minutes consultative discussion and review; wRVU .35 [rates may vary] - 99447, Telephone/Internet Assessment,
11-20 minutes consultative discussion and review; wRVU .7 [rates may vary] - 99448, Telephone/Internet Assessment,
21-30 minutes consultative discussion and review; wRVU 1.05 [rates may vary] - 99449, Telephone/Internet Assessment,
31+ minutes consultative discussion and review; wRVU1.4 [rates may vary]
Guidelines
- The patient for whom the consultation is requested may be either a new patient to the consultant or an established patient with a new problem or an exacerbation of an existing problem.
- The consultant should not have seen the patient in a face-to-face encounter within the last 14 days.
- These codes are not reported when the telephone/Internet/electronic health record consultation leads to an immediate transfer of care or other face-to-face service (e.g., a surgery, a hospital visit, or a scheduled office evaluation of the patient) within the next 14 days or next available appointment date of the consultant.
- Codes 99446, 99447, 99448, 99449, 99451 should not be reported more than once within a seven-day period.
FREQUENTLY ASKED QUESTIONS
- Are there modifiers to CPT codes for telehealth visits?
Yes, there are modifiers. The -95 modifier is appended to a code for a synchronous telemedicine service via real-time interactive audio-visual system. Other payors may use the GT modifier.
Medicare uses place of service of POS 11 (non-facility, higher fee) while commercial payors may use POS 2. - Is there a difference in reimbursement for telephone-only visit (no video)?
Yes. If no video is obtained during the visit, then this would be billed using codes of 99441- 99443. While in the past these visits could only be for follow-up care, effective March 30 these can be used for new patients as well. These codes reimburse at 1.07 wRVU for 99443, so they pay significantly less than the same visit with audio and video.
Important Update: CMS announced on April 30, 2020, that retroactive to March 1, 2020, reimbursements for audio-only telephone evaluation and management telehealth visits will match payments for similar office and outpatient visits, so 99441-99443 phone encounters can be billed at a higher reimbursement rate. - Is there a reimbursement parity between telehealth and face to face visits?
At this current time, Medicare will pay the same for telehealth and face to face visits. The need for a detailed history and physical examination has been eliminated for billing for telehealth visits; you can now bill by time or by medical decision-making complexity. The time includes all the time (in front of the patient and document review) spent on the patient. It does not account for nurse time. Time needs to be documented in the clinical note. - When should consent be obtained for the telehealth visit?
Consent is best obtained at the time the patient makes the appointment and should be documented in the clinical record. - Is there an attestation to a telehealth visit that demonstrates that the visit meets CMS standards?
Suggestion: This telehealth visit was completed with the assistance of an interactive audio/visual real time telecommunication system between the patient and me. The patient consented to participate and received services at (location) while I was located at (location).
The location information is helpful as CMS will not reimburse telehealth visits when the patient is in the same office suite as the provider. - If my virtual visit platform’s audio fails and I use a cellphone for audio and a separate system for video is this OK?
Yes, if both run synchronously. - Can I use Facetime or Skype?
Yes, if this is not a public platform. - Do policies vary by payor?
Yes, several issues differ by payor.- State licensure may be required by other payors but not by Medicare
- Consent for telehealth varies by state especially for State Medicaid programs (See CCHPCA and FSMB links below)
- Telephone calls (no video) are paid significantly less by CMS. This may not be the case with other payors
ADDITIONAL RESOURCES
AES Educational Resources
American Epilepsy Society. Ask the Expert Webinars.
Telehealth for Epilepsy: Overcoming Obstacles. April 3, 2020.
Telehealth in Epilepsy Part 2: Putting Guidelines into Practice. April 20, 2020.
Accessed April 18, 2020.
CMS Medicare Telehealth Resources
Center for Medicare and Medicaid Services. COVID-19 Emergency Declaration Blanket Waivers for Health Care Providers. April 29, 2020. https://www.cms.gov/files/document/summary-covid-19-e mergency-declaration-waivers.pdf. Accessed April 30, 2020.
Center for Medicare and Medicaid Services. Trump Administration Issues Second Round of Sweeping Changes to Support U.S. Healthcare System During COVID-19 Pandemic. April 30, 2020. https://www.cms.gov/newsroom/press-releases/trump-administration-issues-second-round-sweeping-changes-support-us-healthcare-system-during-covid. Accessed May 1, 2020.
Center for Medicare and Medicaid Services. COVID-19 Emergency Declaration Blanket Waivers for Health Care Providers. April 15, 2020. https://www.cms.gov/files/document/summary-covid-19-emergency-declaration-waivers.pdf. Accessed April 20, 2020.
Center for Medicare and Medicaid Services. Clinician Letter. April 7, 2020. https://www.cms.gov/files/document/covid-dear-clinician-letter.pdf. Accessed April 27, 2020.
Center for Medicare and Medicaid Services. Physicians and Other Clinicians: CMS Flexibilities to Fight COVID-19. March 30, 2020. https://www.cms.gov/files/document/covid-19-physicians-and-practitioners.pdf. Accessed April 20, 2020.
Center for Medicare and Medicaid Services. General Provider Telehealth and Telemedicine Tool Kit. [Undated; linked from March 17, 2020 Fact Sheet press release] https://www.cms.gov/files/document/general-telemedicine-toolkit.pdf. Accessed April 18, 2020.
Center for Medicare and Medicaid Services. Medicare Telemedicine Health Care Provider Fact Sheet. March 17, 2020. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet. Accessed April 20, 2020.
Center for Medicare and Medicaid Services, Office of Civil Rights. FAQs on Telehealth and HIPAA during the COVID-19 Nationwide Public Health Emergency. https://www.hhs.gov/sites/default/files/telehealth-faqs-508.pdf. Accessed April 22, 2020.
Center for Medicare and Medicaid Services, Medicare Learning Network. Telehealth Services. March 2020. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/TelehealthSrvcsfctsht.pdf. Accessed April 20, 2020.
CMS Medicaid Telemedicine and Telehealth Resources
Center for Medicare and Medicaid Services. Telemedicine [for Medicaid]. https://www.medicaid.gov/medicaid/benefits/telemedicine/index.html. Accessed April 20, 2020.
Center for Medicare and Medicaid Services. State Medicaid and CHIP Telehealth Toolkit. Policy Considerations for States Expanding Use of Telehealth. COVID-10 Version. April 23, 2020. https://www.medicaid.gov/medicaid/benefits/downloads/medicaid-chip-telehealth-toolkit.pdf. Accessed April 27, 2020.
Telehealth Resources from Other Organizations
American Academy of Neurology. Telemedicine and COVID-19 Implementation Guide. Updated April 10, 2020. https://www.aan.com/siteassets/home-page/tools-and-resources/practicing-neurologist--administrators/telemedicine-and-remote-care/20-telemedicine-and-covid19-v103.pdf. Accessed April 22, 2010.
American Academy of Family Physicians. A virtual visit algorithm: how to differentiate and code telehealth visits, e-visits, and virtual check-ins. In Practice. A Blog from FPM Journal. March 23, 2020. https://www.aafp.org/journals/fpm/blogs/inpractice/entry/telehealth_algorithm.html. Accessed April 18, 2020.
State-Specific Telehealth Requirements
Center for Connected Health Policy. COVID-19 Related State Actions. April 13, 2020. https://www.cchpca.org/resources/covid-19-related-state-actions. Accessed April 18, 2020.
Alliance for Connected Care (ACC)
State Telehealth Expansion (or related expansion which may be relevant for telehealth). April 13, 2020. http://connectwithcare.org/wp-content/uploads/2020/04/Alliance-for-Connected-Care-State-Telehealth-Expansion-by-Governors-Orders-4-13-20.pdf. Accessed April 20, 2020.
1135 State Approvals [chart]. http://connectwithcare.org/wp-content/uploads/2020/04/Approved-1135-State-Waivers-Chart-9-April-2020-1.pdf. April 9, 2020. Accessed April 20, 2020.
[See also other ACC summaries of state telehealth and licensure expansion at: http://connectwithcare.org/state-telehealth-and-licensure-expansion-covid-19-chart/]
Federation of State Medical Boards (FSMB)
States Waiving Telehealth Licensure. April 15, 2020. http://www.fsmb.org/siteassets/advocacy/pdf/states-waiving-licensure-requirements-for-telehealth-in-response-to-covid-19.pdf. Accessed April 20, 2020.
[See also other FSMB summaries of state requirements at: http://www.fsmb.org/advocacy/covid-19/]